The research findings have been published in the renowned scientific journal Cell Metabolism. HKBU researchers will coordinate a phase I and II clinical trial in the Mainland to evaluate the safety and efficacy of HDCA for patients with fatty liver disease and type 2 diabetes.
32% of adults suffer from NAFLD
NAFLD is a leading cause of chronic liver disease, characterised by the build-up of excessive fat in liver cells that is not caused by alcohol consumption. Its global prevalence has been increasing over time. A meta-analysis in 2022 estimated that 32% of the adult population is affected by NAFLD. Some people with NAFLD can develop non-alcoholic steatohepatitis, which is marked by liver inflammation and may progress to cirrhosis and liver failure. Currently, there are no therapeutic drugs available for sale on the market for non-alcoholic steatohepatitis.
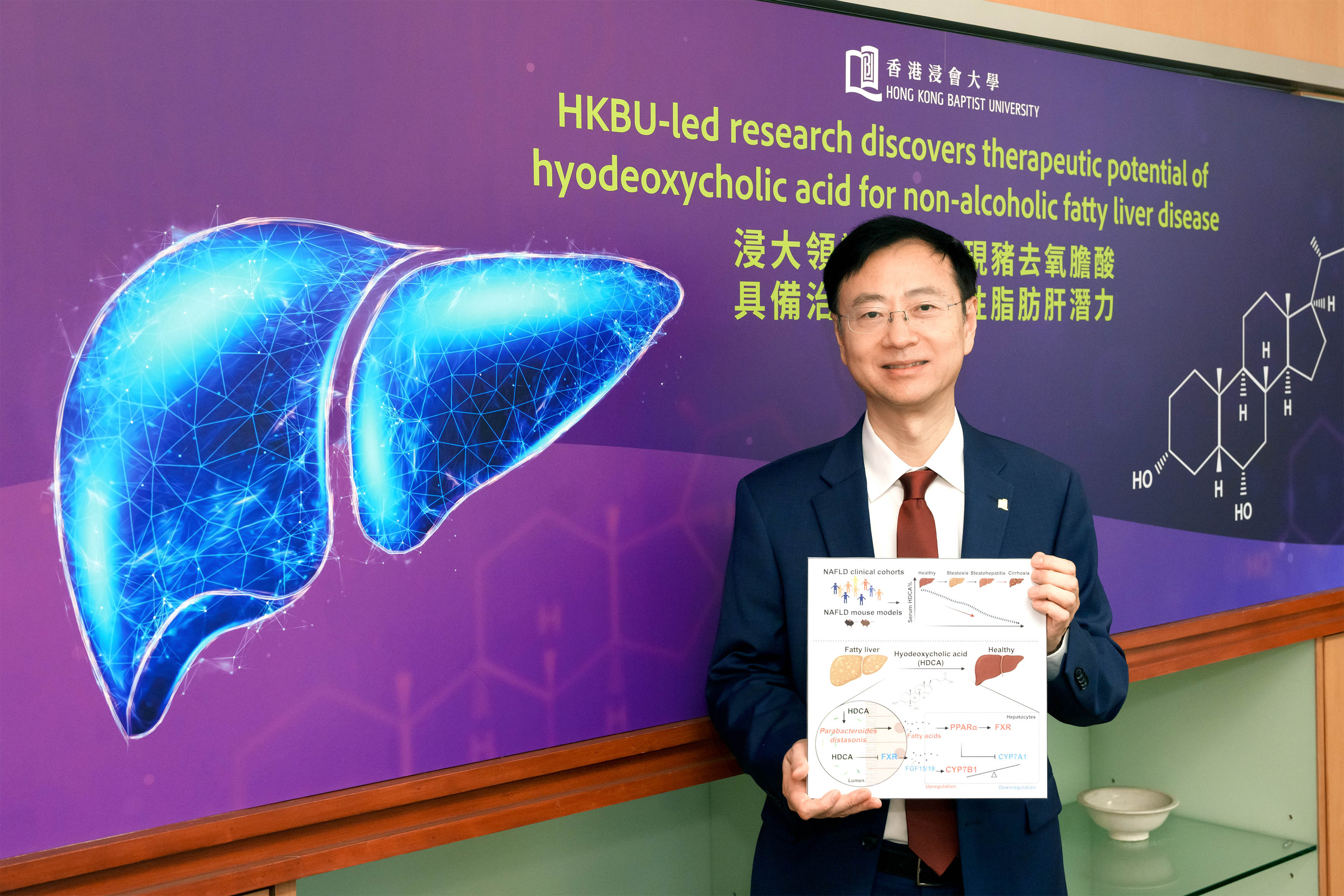
A research led by Professor Jia Wei, Acting Dean and Chair Professor in Chinese Medicine and Systems Biology of the School of Chinese Medicine at HKBU, discovered that HDCA offers promising potential as a pharmaceutical intervention for NAFLD. “Our research is a significant stride forward in understanding the pathophysiology of NAFLD, and it offers a potential new avenue for therapeutic intervention,” he said.
Therapeutic effects of HDCA
Professor Jia’s team found that individuals with NAFLD have lower levels of HDCA compared to those without NAFLD. In a cohort consisting of 178 patients with NAFLD and 73 healthy individuals, hyocholic acid species, including HDCA and its major metabolite glycohyodeoxycholic acid, comprises 0.5% of the bile acids in NAFLD patients, which is significantly lower than the 2% in healthy individuals. This observation led the team to explore HDCA’s potential therapeutic role.
A series of controlled experiments were conducted to evaluate the therapeutic effect of HDCA. The team orally fed HDCA to mouse models with NAFLD for eight weeks. The results showed that HDCA markedly reduced excessive lipid droplets, and improved hepatic inflammation, oral glucose tolerance (i.e. the blood glucose level after oral intake of glucose), and insulin sensitivity (i.e. the sensitivity of the body to the effects of insulin which helps the glucose to enter into the cells for use) compared to the control group. The results revealed that HDCA alleviated NAFLD conditions and the risk factors of NAFLD such as type 2 diabetes and insulin resistance.
Interestingly, the researchers found that HDCA did not exert its therapeutic effects on NAFLD by directly targeting liver cells. They evaluated the potential direct effect of HDCA on lipid accumulation in a mouse model. The results showed that lipid accumulation was barely affected by the HDCA. They hypothesised that HDCA induced gut microbiota alterations, which might contribute to the alleviation of NAFLD.
HDCA reshapes gut microbiota
The researchers observed that HDCA could improve the population of beneficial gut bacteria. Parabacteroides distasonis (P. distasonis), a member of the core microbiome in the human gut, sharply increased in the mouse model fed with high-fat food and administered with HDCA, compared with the control group fed with high-fat food only. The results revealed that HDCA provided a favorable environment for the thriving of P. distasonis, which regulates fatty acid metabolism as well as the hepatic bile acid synthesis pathways.
“The study underscores the crucial role of the gut-liver metabolic axis in disease management. We hope that the research findings on HDCA and the clinical trial to be conducted in the Mainland will provide more insights into the treatment of fatty liver disease and non-alcoholic steatohepatitis,” said Professor Jia.
Professor Jia has also led a research project investigating the molecular connections between metabolic-associated fatty liver disease and type 2 diabetes mellitus, with a specific focus on host-gut microbiota interactions. The project has been awarded over HK$7.2 million in research funding from the Theme-based Research Scheme (13th round) under the Research Grants Council.
Hashtag: #fattyliverdisease
The issuer is solely responsible for the content of this announcement.